(October, 2023) Researchers at the Miami Project to Cure Paralysis are investigating strategies to modify the interactions between the brain and the gut to help patients after stroke as well as Alzheimer’s Disease.
It’s not just a gut feeling.
For at least 15 years, scientists have recognized there is a strong interaction between the brain and the gut. Researchers and clinicians have previously shown that patients who suffer from acute brain injury, such as traumatic brain injury or stroke, often develop gastrointestinal problems.
Importantly, new research at the Miami Project to Cure Paralysis, a Center of Excellence at the Miller School of Medicine, indicates that there is a bidirectional relationship between the brain and the gut. This means that people with existing gut conditions—like colitis or irritable bowel syndrome—may exhibit an increased vulnerability to develop a neurodegenerative condition like Alzheimer’s Disease or cerebrovascular disorders such as stroke. Interestingly, people with existing neurological conditions like Alzheimer’s Disease, or who have suffered a stroke, are also more likely to develop gut related disorders.
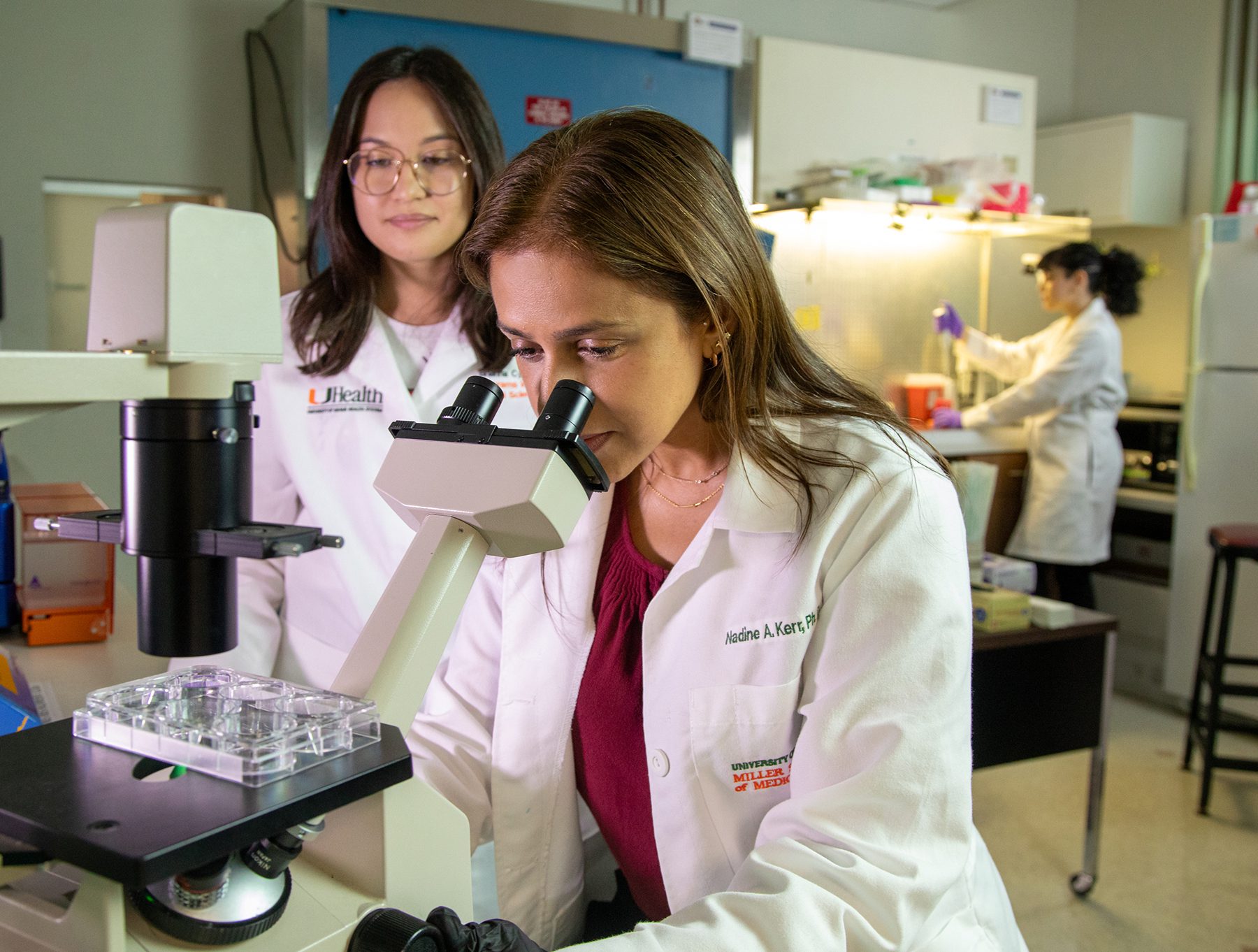
Since stroke remains the second leading cause of death worldwide and Alzheimer’s Disease impacts more than 10 percent of Americans over 65, a team at the Miami Project is actively working to understand the gut-brain connection in clinically relevant models. Toward that goal, Dr. Nadine Kerr, a Research Assistant Professor of Neurological Surgery and The Miami Project, recently received a grant from the Alzheimer’s Association to look for a way to critically study what is called the bidirectional gut-brain-axis after stroke in an AD genetic pre-clinical model.
“Patients with Alzheimer’s Disease are more susceptible to stroke and can also suffer from gut disorders. We therefore proposed to examine how the bidirectional gut-brain-axis plays a role in the development of Alzheimer’s Disease after stroke and long-term consequences,” said Kerr, who received the three-year, $250,000 grant as a young investigator. “Targeting underlying mechanisms could improve the quality of life for patients with chronic gut complications from developing Alzheimer’s disease or having a stroke.”
Importantly, Kerr emphasizes the need to critically study and understand this process because studied have shown that chronic gut problems, such as constipation, are found to be more prone to accelerated cognitive decline.
“After stroke or getting Alzheimer’s Disease, people with gut problems often end up with worsened neurological outcomes, which is one of the main reasons why we chose to study the bidirectional communication between these organs,” she said.
In particular, Kerr’s team is focused on how proteins called inflammasomes are transported from the brain to the gut via extracellular vesicles, which are small particles released from various cell types into bodily fluids (i.e. blood, cerebrospinal fluid, and stool). This inflammatory response can happen within the first few days after a stroke. Additionally, in people diagnosed with Alzheimer’s Disease there is a known increase in inflammasome activation in the brain and gut. Typically, once inflammasome pathways are activated, a process called pyroptosis is triggered, a form of cell death that occurs in the brain and the gut. In 2022, the team published a paper that found that pyroptosis plays an important role in disruption of the gut-brain axis after stroke. In this grant, they aim to further understand this mechanism in the context of Alzheimer’s Disease and stroke. By understanding the significance of this process, Kerr believes that her team may be able to study therapeutic drugs that could target the transfer of these inflammasomes to the gut, and potentially help patients who have experienced stroke or Alzheimer’s Disease to avoid further systemic organ complications and progression of neurological deficits.
“Targeting extracellular vesicle signaling and pyroptotic cell death are mechanisms we are hoping to clarify that could lead to therapeutic interventions and biomarkers for the treatment and diagnosis of gut-brain axis complications after CNS injury” she said. “And if we could do that, it could also likely improve a patient’s long-term neurological conditions, so there is less cognitive decline and gut complications.”
But their work could also benefit other CNS disorders, Kerr notes, because it could allow clinicians to better understand how the brain communicates with the gut. Lifestyle changes, such as altering one’s diet, improving the health of the gut microbiome, may help to reduce further gut complications in patients with neurological disease.
“I’m sure most people have had some gut issues, whether it is diagnosed or not,” Kerr said. “The health of the gut is dependent on what we eat as well as other factors, studying how the brain and the gut interact and can be modified is really important.”
Kerr’s team science program includes Dr. Helen Bramlett, Professor of Neurological Surgery, Dr. W. Dalton Dietrich, Scientific Director of the Miami Project and Professor of Neurological Surgery, Dr. Juan Pablo de Rivero Vaccari, Associate Professor of Neurological Surgery and Dr. Robert W. Keane, Professor of Physiology and Biophysics.
By Janette Neuwahl Tannen