(December, 2023) The Miami Project’s Jonathan Jagid, M.D. and Brian Noga, Ph.D., have a proven history of working together on deep brain stimulation (DBS) for movement. Now the robust expertise they built through The Miami Project is poised to impact various neurological conditions including walking after spinal cord injury (SCI). Concurrently the DBS program, routinely used for treatment of “freezing of gait”, or “FOG”, in people with Parkinson’s, is now on the verge of a remarkable translation into the realm of SCI, offering newfound hope for regaining the ability to walk.
Parkinson’s disease, a progressive neurodegenerative disorder, can result in FOG characterized by momentary immobility despite intent to move. Traditional treatments, including medications and DBS, have offered relief to many, but some individuals remain unresponsive to these approaches. Deep Brain Stimulation (DBS), a surgical technique involving the implantation of electrodes into specific brain regions, initially garnered attention for its remarkable success in alleviating FOG in Parkinson’s patients.
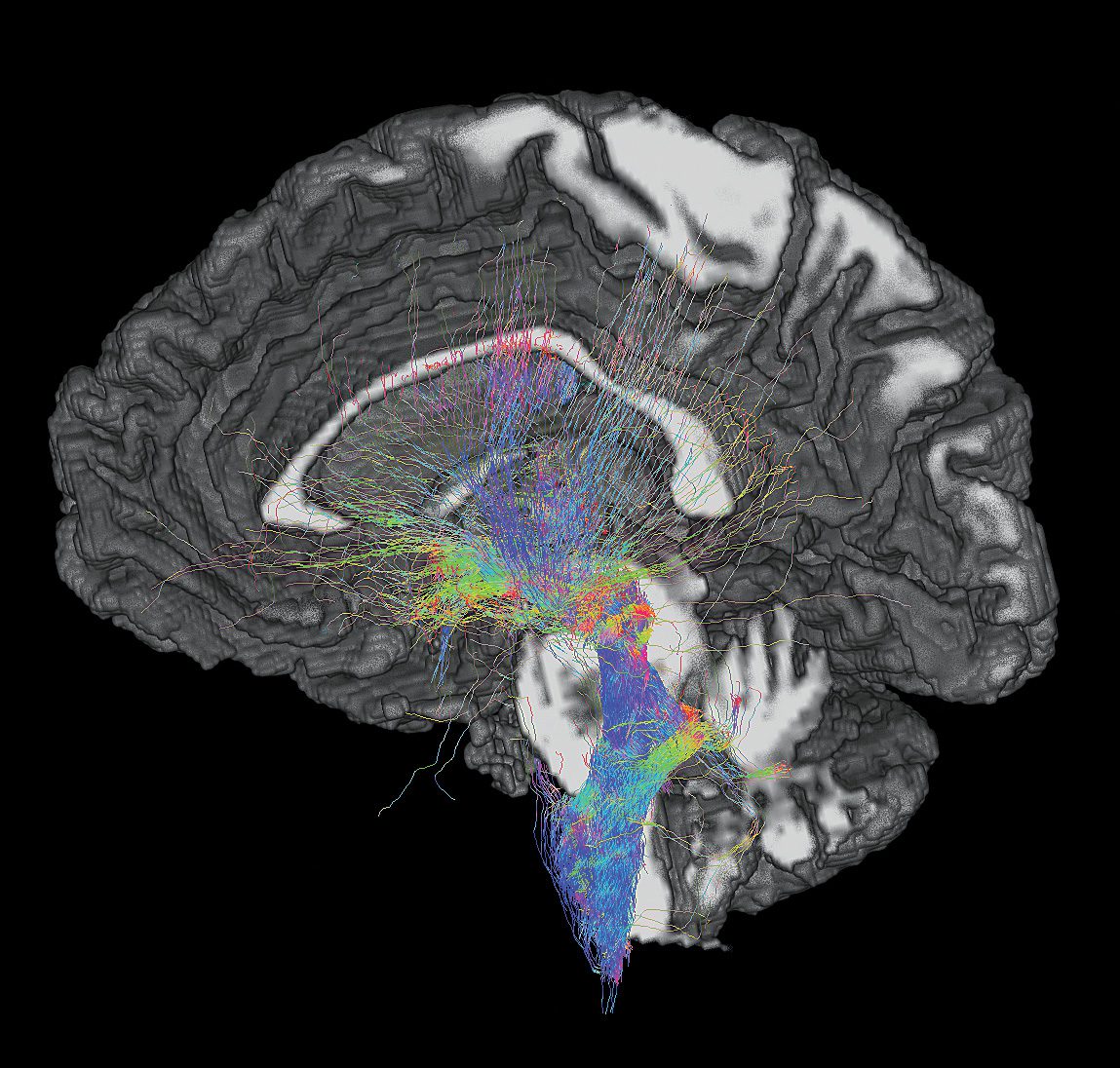
By modulating neural activity in targeted areas, DBS effectively unlocks frozen feet. However, there are important scientific questions on where to stimulate, engineering questions of how to deliver just the right amount of electricity to the area, and surgical questions of how to safety and reliably deliver the probes to their target areas in the brain.
Dr. Jagid’s DBS program has optimized the implementation of DBS for FOG, and Dr. Noga’s pre-clinical research has separately identified the brain and spinal circuitry responsible for the control of walking. Together, they now have the potential to translate the success of DBS in Parkinson’s into a therapeutic beacon for SCI patients.
The key to their quest lay in the intricacies of the brain’s mesencephalic locomotor region (MLR), a neural hub responsible for orchestrating locomotion. While the MLR’s anatomical complexity presented challenges, it also held the promise of a breakthrough. As outlined in a recent scientific review published by Dr. Noga, pioneering studies have shown the MLR’s importance in controlling walking in many different models of SCI.
Previous DBS studies had implicated the cuneiform nucleus (CnF), a region within the MLR, as a potential target for promoting gait initiation. However, traditional DBS for FOG has targeted different brain regions. Thus Drs. Jagid and Noga and their colleagues have set out on a protocol for an ongoing prospective pilot clinical trial using direction DBS probes to target the CnF in FOG. This trial is an optimization of an existing approach, shifting the location of the DBS probe placement to the CnF and using a directional probe that has a circular lead architecture that allow for steering of the current to hit only the CnF and avoid activation of off-target brain regions. Having implanted multiple participants in this study, the study team is confident in their equipment and approach. Combined with this success in FOG and their knowledge of the role the CnF plays in walking post-SCI, the stage is set to assess the safety, feasibility, and efficacy of CnF DBS in individuals with incomplete SCI.
In the realm of neurosurgery, the journey from Parkinson’s to paralysis has been a remarkable one. What has been learned about DBS in Parkinson’s patients grappling with FOG now seems to hold the potential to translate into walking after SCI. The story is far from over, but with each step, we are brought closer to a future where mobility is within reach for all those affected by paralysis.